Shock is a life-threatening condition that occurs when the body does not have adequate blood flow. A lack of blood flow means that cells and organs do not get enough oxygen and nutrients to function properly. This can result in multiple organ damage. Concussion requires immediate treatment and can get worse very quickly. Trauma, in physiology, is the failure of the circulatory system to supply adequate blood to the peripheral tissues to meet the basic metabolic needs of oxygen and nutrients and the incomplete removal of metabolic wastes from the affected tissue. Shock is usually caused by hemorrhage or excessive infection and in most cases is caused by a weak, rapid pulse. low blood pressure; and cold, sweaty skin.Shock Disease

Depending on the cause, however, some or all of these symptoms may be absent in individual cases. Psychotic shock is caused by a traumatic event and is also called acute stress disorder. This type of shock causes a strong emotional response and can also cause physical reactions. This article focuses on the multiple causes of physiologic shock. Your body goes into shock when your system doesn’t have enough blood circulation to keep organs and tissues functioning properly. It can be caused by any injury or condition that affects blood flow in your body. Trauma can lead to multiple organ failures as well as life-threatening complications. Shock Disease
Major Types and Causes of Shock Disease
There are four major types of concussions, each of which can be caused by different events.
Obstructive shock Disease
Obstructive shock happens when blood can’t get to where it needs to go. Pulmonary embolism is a condition that can cause blockage of blood flow.
Conditions that can cause air or fluid to build up in the chest cavity can also lead to obstruction. These include:
- Pneumothorax (collapsed lung)
- Cardiac tamponade
Cardiogenic Shock
Damage to your heart can reduce the blood flow to your body, which can lead to cardiogenic shock. Common causes of cardiogenic shock include:
- Damage to your heart muscle
- Irregular heart rhythm
- Very slow heart rate
Splitting shock
Conditions that reduce the tone of your blood vessels can cause distributive shock.
Unprovoked shock can result in symptoms that include:
- Flushing
- Low blood pressure
- Loss of consciousness
There are many types of distribution shocks, including:
Anaphylactic shock is a complication of a severe allergic reaction known as anaphylactic. An allergic reaction occurs when your body mistakes a harmless substance for something harmful. It triggers a dangerous immune response. Anaphylactic is usually caused by an allergic reaction to food, insect venom, medication, or latex.
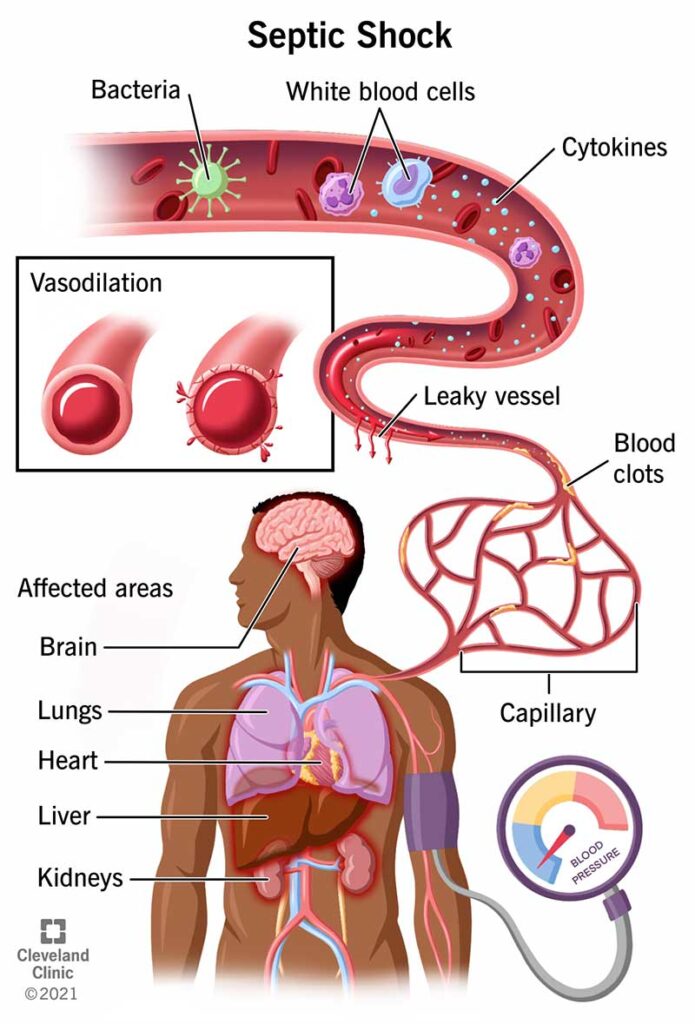
Septic shock is another form of distributive shock. Sepsis also called blood poisoning, is a condition caused by an infection that leads to bacteria in your blood. Septic shock occurs when bacteria and their toxins cause severe tissue or organ damage in your body.
Neurogenic shock is caused by damage to the central nervous system, most commonly a spinal cord injury. This causes the blood vessels to dilate, and the skin can feel hot and sticky. The heart rate slows, and the blood pressure drops dramatically.
Hypovolemic shock occurs when your blood vessels have no enough blood to carry oxygen to your organs. This can be caused by severe loss of blood, for example, from injuries. So your blood delivers oxygen and other vital nutrients to your organs. If you lose too much blood, your organs may not function properly. Severe dehydration can also lead to this type of shock.
Signs and Symptoms of Shock Disease
Signs and symptoms of shock disease may vary depending on the situation and may include:
- Cold, clammy skin
- Pale or ashy skin
- Bluish color (or gray in case of black discoloration) on the lips or nails.
- Rapid pulse
- Breathing fast
- Nausea or vomiting
- Dilated pupils
- Weakness or fatigue
- Dizziness or fainting
Emergency Medical Care.
Call 911 or your local emergency number if you suspect that someone is in shock. Then immediately take the following steps:
- Have the person lie down and elevate the legs and feet slightly, unless you think this may cause pain or further injury.
- Keep the person still and do not move unless absolutely necessary.
- Start CPR if the person shows no signs of life, such as not breathing, coughing, or not moving.
- Loosen tight clothing and, if necessary, cover the person with a blanket to prevent exposure to cold.
- If you suspect the person has an allergy, and you have access to an epinephrine auto-injector, use it according to their instructions.
- If the person is bleeding, apply pressure to the bleeding area using a towel or sheet.
- If the person vomits or starts bleeding from the mouth, and no spinal cord injury is suspected, turn them to one side to prevent suffocation.
How is Trauma Diagnosed?
First responders and doctors often recognize trauma by its outward symptoms. They can also check:
- Low blood pressure
- Weak pulse
- Fast heartbeat
Once they are diagnosed with shock, their first priority is to provide life-saving treatment to get the blood circulating as quickly as possible. This can be done by giving fluids, medications, blood products, and supportive care. It will not be resolved until they can find and treat the cause.
Once you’re stabilized, your doctor can try to diagnose the cause of the shock. To do this, they may order one or more tests, like imaging or blood tests.
Imaging test
Your doctor may order imaging tests to check for injury or damage to your internal tissues and organs, like:
- Fracture of bones
- Rupture of organ
- Muscle or tendon tears
- Abnormal growth
Such tests include:
- Ultrasound
- X-ray
- CT scan
- MRI scan
- Blood tests
Your doctor may use blood tests to look for these symptoms:
- Significant blood loss
- Infections in your blood
- Drug or medication overdose
Medical care
Your doctor’s treatment plan for trauma will depend on the cause of your condition. Different types of shock are treated differently. For example, your doctor may use:
- Epinephrine and other medications to treat anaphylactic shock
- Blood transfusions to replace lost blood and treat hypovolemic shock
- Medications, heart surgery, or other interventions to treat cardiogenic shock.
- Antibiotics to treat septic shock

