This is the term given to heart problems caused by narrowed arteries of the heart. Once the arteries area unit narrowed, less blood and element reach the guts muscle. it’s conjointly known as artery unwellness and coronary cardiopathy. This may eventually cause heart failure. But cardiac muscle anemia, conjointly called internal organ anemia, reduces the guts muscle’s ability to pump blood. A sudden, severe blockage of 1 of the heart’s arteries will cause heart failure. cardiac muscle anemia also can cause serious abnormal heart rhythms. Treatment of cardiac muscle anemia involves rising blood flow to the guts muscle. Treatment might embrace medications, a procedure to open blocked arteries (angioplasty), or bypass surgery. Creating wholesome lifestyle selections is vital for the treatment and hindrance of cardiac muscle anemia. Ischemic Disease
The term anemia cardiopathy (IHD) describes a bunch of clinical syndromes characterized by cardiac muscle anemia. The associated an imbalance between cardiac muscle blood offer and demand. A result of the first pathophysiologic defect in anemia heart muscle is the insufficient introduction. Anemia is associated not solely with lean element delivery but conjointly with reduced accessibility of nutrients and inadequate excretion of the metabolic finish product. In cardiac muscle anemia, the results of element deprivation can not be separated from the consequences of impaired matter washout. In conditions related to isolated hypoxemia and preserved introduction (such as cyanotic nonheritable cardiopathy, severe anemia, or advanced respiratory organ disease), the injurious consequences for the heart muscle area unit are sometimes less pronounced, resulting in the elimination of metabolites and metabolic substrates. Highlight the importance of providing the pathologic process of anemia injury. Ischemic Disease
Silent Ischemia
Many Americans may be having ischemic episodes without knowing it. These people have painless ischemia, i.e. silent ischemia. They can have a heart attack without warning. Undiagnosed episodes of silent ischemia may also occur in people with angina. In addition, people who have had previous heart attacks or who have diabetes are particularly at risk of developing silent ischemia.
Symptoms of Ischemic Disease
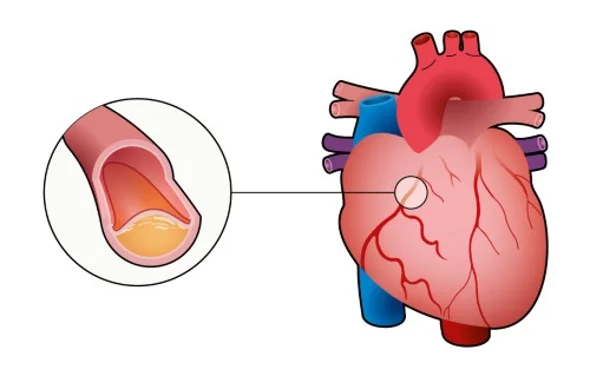
Myocardial ischemia occurs when blood flow through one or more of your coronary arteries is reduced. Reduced blood flow reduces the amount of oxygen your heart muscle gets.
Myocardial ischemia can develop slowly as the arteries close over time. Or it can happen quickly when an artery suddenly closes.
Conditions that can lead to myocardial ischemia include:
- Coronary artery disease (atherosclerosis). Plaque, made mostly of cholesterol, builds up on the walls of your arteries and restricts blood flow. Atherosclerosis is the commonest cause of myocardial ischemia.
- Blood Clot Plaques that form in atherosclerosis can rupture, causing blood clots. A clot can block an artery and cause sudden, severe myocardial ischemia, resulting in a heart attack. Rarely, a blood clot can travel to a coronary artery from elsewhere in the body.
- Coronary artery spasm. This temporary hardening of the muscle in the artery wall can briefly decrease or block blood flow to the heart muscle. Coronary artery spasm is the most common cause of myocardial ischemia.
Chest pain associated with myocardial ischemia may be caused by:
- Physical exertion
- Emotional stress
- Cold temperature
- Cocaine use
- Eating heavy or large meals
- Sexual intercourse
Causes of Ischemic Disease
Some people have silent ischemia of the heart or brain. This is when you have ischemia but have no pain or other signs or symptoms. This can lead to a heart attack or stroke that seems out of the blue.
If you get symptoms, they vary based on where you have ischemia. Here are the areas where ischemia can occur and the symptoms you may experience:
Heart
- Chest pain (angina)
- A heartbeat that is faster than normal.
- Shortness of breath while exercising
- Sweating when you least expect it.
- Upset stomach or throwing up
- too tired
Brain
- Headaches that are severe and sharp, sometimes with dizziness or lightheadedness
- is passing
- Difficulty moving your body (weakness, numbness, or you can’t move your face, arm, or leg to one side of your body)
- Slurred speech and difficulty understanding others
The legs
- Coldness and weakness in your feet
- Pain in your legs
- Severe pain in your legs even while resting
- Glowing, smooth skin on your legs and feet
- Wounds that won’t heal.
Intestines
- Severe abdominal pain
- Bloating
- Blood in your poop
- Diarrhea
- Stomach upset or upset stomach
Prevention of Ischemic Disease
You can help reduce the chance of ischemia by making healthy lifestyle choices. These include:
- Eat more fruits, vegetables, and whole grains
- Exercise frequently
- Reducing your stress and try deep breathing, meditation, or yoga
- Quit smoking
- Keeping track of your other health problems, such as diabetes, high blood pressure, and high cholesterol
They can check for problems like high blood pressure, high cholesterol, and diabetes. This can help you catch problems early before symptoms appear.
Diagnosis of Ischemic Disease
Your doctor will start by asking questions about your medical history and performing a physical exam. After that, your doctor may prescribe:
- Electrocardiogram (ECG). The electrodes attached to your skin record your heart’s electrical activity. Some changes in your heart’s electrical activity can be a sign of heart damage.
- Pressure check. Your heart rate, blood pressure, and breathing are monitored while you walk on a treadmill or ride a stationary bike. Exercise makes your heart pump harder and faster than usual, so a stress test can detect heart problems that might otherwise go unnoticed.
- Echocardiogram. Sound waves directed at your heart from a wand-like device placed on your chest produce video images of your heart. So an echocardiogram can help identify if a part of your heart is damaged and not pumping normally.
- Stress Echocardiogram. A stress echocardiogram is similar to a regular echocardiogram, except you exercise in the doctor’s office on a treadmill or stationary bike.
- Nuclear Stress Test. Very small amounts of radioactive material are injected into your bloodstream. When you exercise, your doctor can see the blood flow through your heart and lungs – allowing blood flow problems to be identified.
- Coronary Angiography. A dye is inserted into your heart’s blood vessels. A series of X-ray images (angiograms) are then taken, showing the path of the dye. This test gives your doctor a detailed look inside your blood vessels.
- Cardiac CT Scan. This test can determine if you have calcium deposits in your coronary arteries – a sign of coronary atherosclerosis. The arteries of the heart can also be seen using CT scanning (coronary CT angiogram).
Treatment
The goal of treatment for myocardial ischemia is to improve blood flow to the heart muscle. Depending on the severity of your condition, your doctor may prescribe medication, surgery, or both.
Medicines
Medications to treat myocardial ischemia include:
- Aspirin. Daily aspirin or another blood thinner can reduce your risk of blood clots, which can help prevent blockages in your coronary arteries. Ask your doctor before you start taking aspirin as it may not be suitable if you have a bleeding disorder or if you are already taking another blood thinner.
- Nitrates. These drugs widen the arteries, improving blood flow to your heart. Improved blood flow means your heart doesn’t have to work as hard.
- Beta-blockers. These drugs help relax your heart muscle, slow your heart rate, and lower your blood pressure so that blood can flow more easily through your heart.
- Calcium channel blockers. These drugs relax and widen blood vessels, increasing blood flow to your heart. Calcium channel blockers also slow your heart rate and reduce the workload on your heart.
- Cholesterol-lowering drugs. These drugs reduce the plaque material that builds up in the coronary arteries.
- Angiotensin-converting enzyme (ACE) inhibitors. These medicines help to relax the blood vessels and lower blood pressure. If you have high blood pressure or diabetes in addition to myocardial ischemia, your doctor may recommend an ACE inhibitor. ACE inhibitors may also be used if you have heart failure or if your heart does not pump blood effectively.
- Ranolazine (Ranexa). This medicine helps relax your coronary arteries to reduce angina. Ranolazine may be prescribed in combination with other angina medications, such as calcium channel blockers, beta-blockers, or nitrates.
Procedures to improve blood flow
Sometimes, more offensive treatments are needed to improve blood flow. Procedures that may help include:
- Angioplasty and stenting. A long, thin tube called a catheter is inserted into the narrowed part of your artery. A wire with a small balloon is inserted into the narrowed area and inflated to widen the artery. So usually, a small wire mesh coil (stent) is inserted to keep the artery open.
- Coronary artery bypass surgery. A surgeon creates a graft using a vessel from another part of your body that allows blood to flow around a blocked or narrowed coronary artery. But this type of open heart surgery is usually only used for people with very narrow coronary arteries.
- Improved external anti-pulsation. This non-invasive outpatient treatment may be recommended if other treatments don’t work. The cuffs wrapped around your legs are gently inflated with air and then deflated. So the pressure on your blood vessels can improve blood flow to the heart.

